Of all the structures of the heart to image with echocardiography, few are as challenging as the mitral valve. Adding to this complexity is the strong support for mitral valve repair in patients with non-ischemic mitral valve disease. It is fair to say that having an excellent command of how to evaluate a mitral valve in the perioperative period is a valuable skill.
Before you can perform a complete mitral valve exam, you need to understand the complex anatomical structure of the mitral apparatus. Here is a quick review of the basic anatomy before we dive into how to perform a complete mitral valve exam with ttransesophageal echo.
The mitral valve apparatus includes six components:
- A fibrous skeleton
- A mitral annulus
- Two mitral leaflets
- Two papillary muscles
- Numerous chordae tendinae
- The left ventricle
The Annulus:
The mitral annulus is a saddle-shaped ring which forms the attachment site for the mitral valve leaflets. The annulus will decrease in the area as it descends towards the left ventricular apex during systole. The mitral annulus fibrosus is formed by the lateral extensions of fibrous tissue from the left and right fibrous trigones. The amount of fibrous tissue decreases as it wraps around the posterior leaflet until only myocardium is present. The lack of fibrous tissue makes the posterior mitral annulus more prone to annular dilation.
Mitral Annulus Anatomic Points:
- The highest point of the saddle is the shorter axis of the mitral annulus and is imaged best in the ME LAX.
- The lower (closer to the LV Apex) point of the saddle is along the longer axis of the annulus and is imaged in the ME commissural view.
- Because of these differences, the mitral valve annulus should be measured at end-systole in both the ME commissural and LAX views.
ECHO KEY POINT: The diagnosis of MVP should only be made in reference to the upper axis in the ME LAX
The Leaflets
The mitral valve is a bicuspid valve with two very distinct and different leaflets.
Anterior Leaflet:
The anterior leaflet is adjacent to the fibrous trigone and the aortic valve. It has a narrow annular attachment to approximately one-third of the mitral annular circumference. The anterior leaflet does have a much longer leaflet length.
Posterior Leaflet:
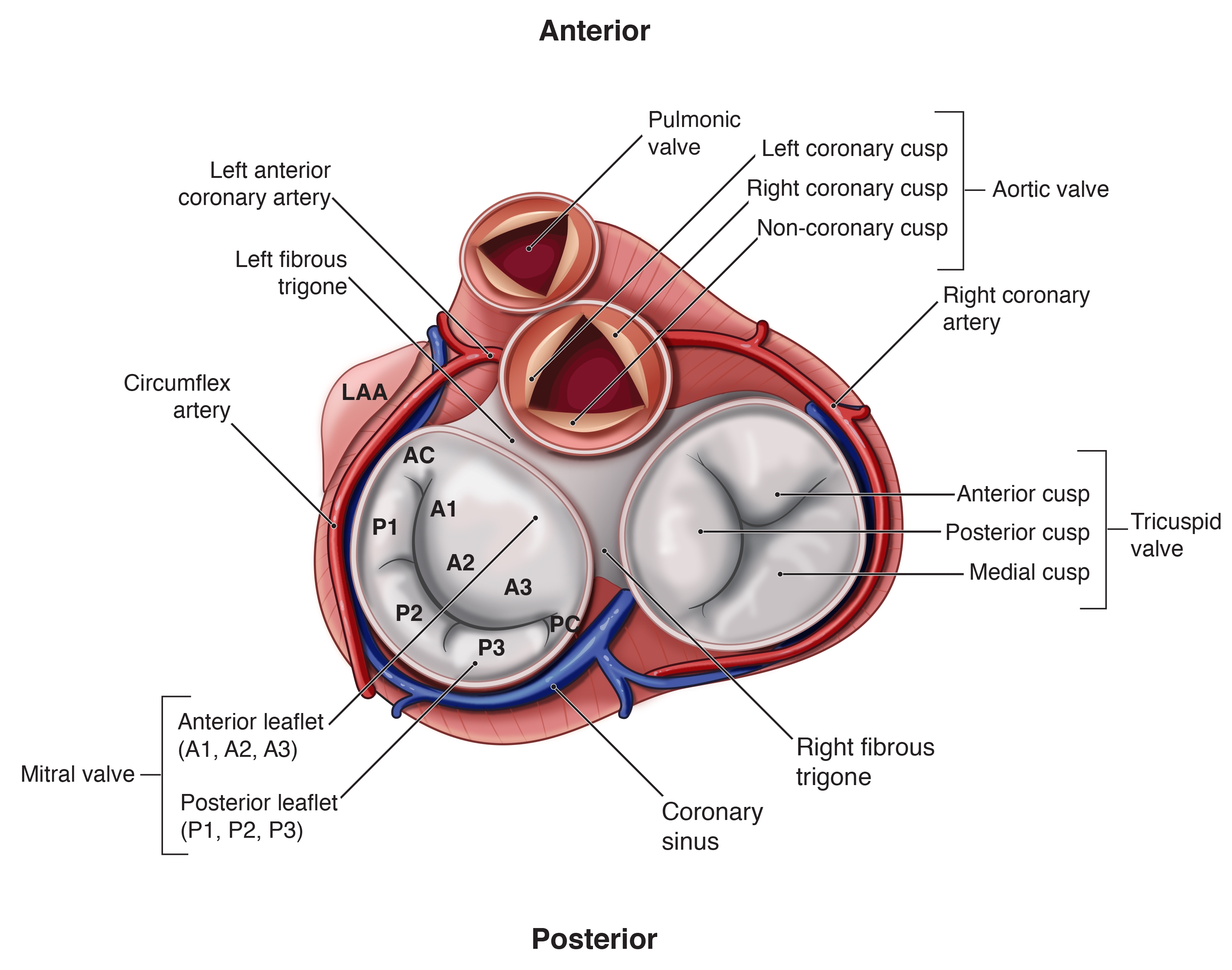
Compared to the anterior leaflet, the posterior leaflet has twice as much annular attachment. It comprises up to two-thirds of the mitral annular circumference and is much narrower than the anterior leaflet. The posterior leaflet is also divided into 3 distinct scallops with the scallop closest to the left atrial appendage and the anterolateral commissure named the P1 segment.
Although they are shaped quite differently, the two leaflets have similar surface areas. The two leaflets join at the anterolateral and the posteromedial commissures. Normal mitral valve function requires good
The Carpentier nomenclature has been used in the ASE / SCA guidelines and is the nomenclature I have seen most commonly used clinically. In this nomenclature, the anterior leaflet is named in segments corresponding to the posterior scallops: A1/P1 is considered the lateral scallop, A2/P2 the middle scallop, A3/P3 the medial scallop.
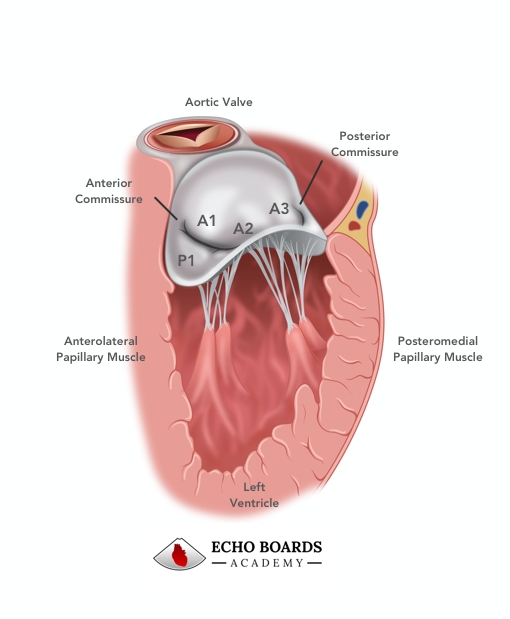
The Papillary Muscles and Chordae T endineae
The two papillary muscles and numerous chordeae tendinae comprise the subvalvular apparatus and support the mitral valve.
- The anterolateral papillary muscle supports the anterolateral segments of each leaflet, Carpentier A1/P1, and A2/P2 scallops.
- The posteromedial papillary muscle is close to the interventricular septum and supports the posteromedial segments of the leaflets, Carpentier A3/P3, and A2/P2
s callops.
KEY POINT: The anterolateral papillary muscle has dual blood supply from the LAD and circumflex coronary arteries. The posteromedial is usually supplied by a single coronary artery. This is most commonly from a branch off the posterior descending artery (an extension of the right coronary artery) or less commonly a branch from an obtuse marginal artery ( a branch of the circumflex artery)
The Left Ventricle
Last but not least, the left ventricular myocardium can affect the function of the mitral valve, changing the position of the papillary muscles and changing the mitral valve coaptation point. The most common example of this is the dilated left ventricle which pulls the coaptation point deeper, causing leaflet tethering.
The Orientation of the Mitral Valve
There are three main orientations for the mitral valve. The anatomic view, as viewed from the base of the heart. The TEE view and the Surgeons view.
The Standard Mitral Valve Exam
A systematic exam of the mitral valve based on the ASE / SCA guidelines consists of four ME views, and two transgastric views. To be a good Echocardiographer, you will need to be able to relate your EchoViews to a specific anatomic location of the mitral valve. 3d TEE is making it easier to demonstrate an anatomically accurate view of mitral valve pathology, however, without good 2D images, you cannot have a good 3D image.
There is a large amount of confusion about which mitral segments you are viewing on the mid-esophageal views. This is because you can obtain views of multiple different segments from the same
- your probe depth (withdraw/advance),
- rotating the probe (clockwise/
counter clockwise ) - or flexing/
retroflexing the probe
In general, when preparing for your echo boards, it’s best to use the segments listed on the standard views of ASE / SCA guidelines.
The ASE / SCA guidelines can be found here and recommend :
- ME four-chamber view for the A3 / P1 scallops
- ME mid-commissural view for P3 / A2 / P1 scallops
- ME anterior-commissural view for A3 / A2 / A1
- ME posterior-commissural view for P3 / P2 / P1
- ME two-chamber view for P3 / A1
- ME long-axis view for A2 / P2
- Transgastric basal short-axis view
- Transgastric two-chamber view
The Exam proposed by Foster et al recommends the following views to evaluate the different mitral segements:
- ME five-chamber view A1 / P1
- ME four-chamber view A2 / P2
- ME four-chamber view A3 / P3
- ME mid commissural view P3 / A2 / P1
- ME anterior-commisural view A3 / A2 / A1
- ME posterior-commissural view P3 / P2 / P1
The Exam proposed by Lambert et al recommends the following views to evaluate the different mitral segments.
- ME five-chamber view A1-2 / P1-2
- ME four-chamber view A2-3 / P2-3
- ME two-chamber view anterior P3 / A2-3
- ME two-chamber view
mid P3 / A2 / P1 ( this is the same as mitral commissural view ) - ME two-chamber view (post) P3 / P2 / P1 ( this is the same as the mitral commissural view )
Clinically, the purpose of your exam is to identify each of the components of the mitral valve and determine their contribution to any mitral valve dysfunction. Continue reading to see how we recommend performing a complete mitral exam.
ME Four-Chamber
The exam begins in the ME Four-Chamber View. Your omniplane angle can range between 0 – 20 degrees for an optimal view. As an experienced echocardiographer, you can visualize most of the mitral segments from this one view. The challenge is confirming which segment you see your with your other views that offer another view of specific segments. Think of it as getting a second opinion.
The standard four-chamber view shows the A2 / P2 scallops along with the posterior scallops of the tricuspid valve. A common finding in this view is the P2 prolapse.
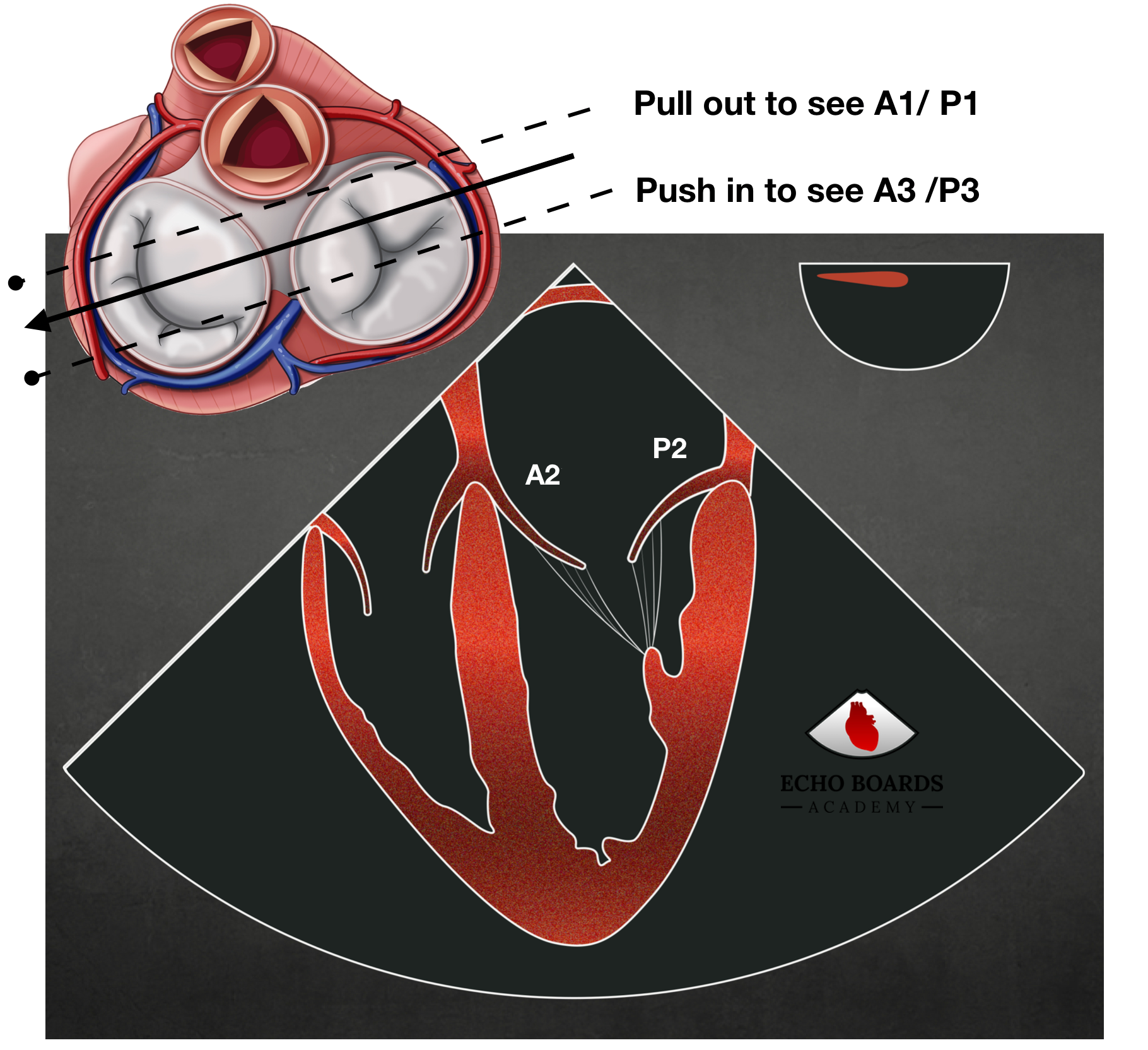
If you withdraw or place anteflexion on the probe slightly you are directing your view more anterior. You will observe:
- more likely getting the A1 / P1 segments.
- the disappearance of the tricuspid valve leaflets
- occasionally the appearance of the LVOT and aortic valve leaflets
If you advance the probe or place retroflexion on the probe you are directing your view more posterior and likely viewing the A3 / P3 segments. If you continue to advance you will lose the mitral valve leaflets and see just the tricuspid valve.
ME Commissural
The mid-esophageal commissural view can be found anywhere between 30-90 degrees on the omniplane angle depending on the rotation of the heart. The ASA / SCA standard ME commissural view runs along the low, long axis of the mitral valve and brings both the anterior and posterior commissures and papillary muscles into view. In this view, you will find from left to right on your screen the P3 / A2 / P1 segments.
If you rotate your probe clockwise towards the right you bring more of the anterior mitral segments into view. Here you will see the A3 / A2 / A1 segments.
If you rotate your probe counterclockwise towards the left, you bring more of the posterior segments into view. Here you will see the P3 / P2 / P1 segments.
ME Two-Chamber
As you continue to advance your omniplane angle you get the mid esophageal two-chamber view. This is typically found between 80-110 degrees on the omniplane. In this view, you catch the left atrial appendage and a large portion of the anterior leaflet with a small part of the P3 segment. If you remember that the A1 / P1 segments arise laterally closest to the left atrial appendage, you can see how you are at times looking down the entire anterior leaflet down towards the P3 segment.
ME Long Axis
Once you have imaged the segments in the ME two-chamber view, continue to rotate your omniplane angle to the 110-135 degree angle. Here you bring the long axis of the aortic valve and the LVOT into view. This view cuts the mitral valve along the high short axis and the A2 / P2 scallops. This is also the view that you want to use to look for mitral valve prolapse since it represents the highest point of the mitral valve annulus.
TG Basal Short Axis
Once you have completed your exam in the mid esophageal views, advance your probe into the stomach and obtain the basal transgastric view. In this view, the anterior leaflet is on the left side of your screen and the posterior leaflet on the right side of your screen. This view is useful for :
- looking for clefts or perforations in the mitral valve
- localizing a mitral regurgitation jet with color flow doppler
- Mapping a mitral valve area although it may be inaccurate because the beam doesn’t always cut perpendicular to the valve.
TG Two-Chamber
Once the basal transgastric view is obtained. relax the flexion slightly and rotate the omniplane angle to 90 degrees to form the transgastric short-axis view. This view is best used for imaging the subvalvular apparatus of the mitral valve with both papillary muscles usually seen along with the primary, secondary and tertiary chordae tendinae.
KEY POINT: When imaging the MV, reduce your sector depth and adjust your focus to concentrate on the MV once you have an overall assessment of the LV size and function.
Additional Modalities:
In each view the mitral valve should be examined with:
- 2-D imaging color flow Doppler
- transmitral Doppler waveforms
- pulmonary veins Doppler waveforms
- 3-D echocardiography
These are best explained when imaging pathology and will be explored in more detail in other sections.